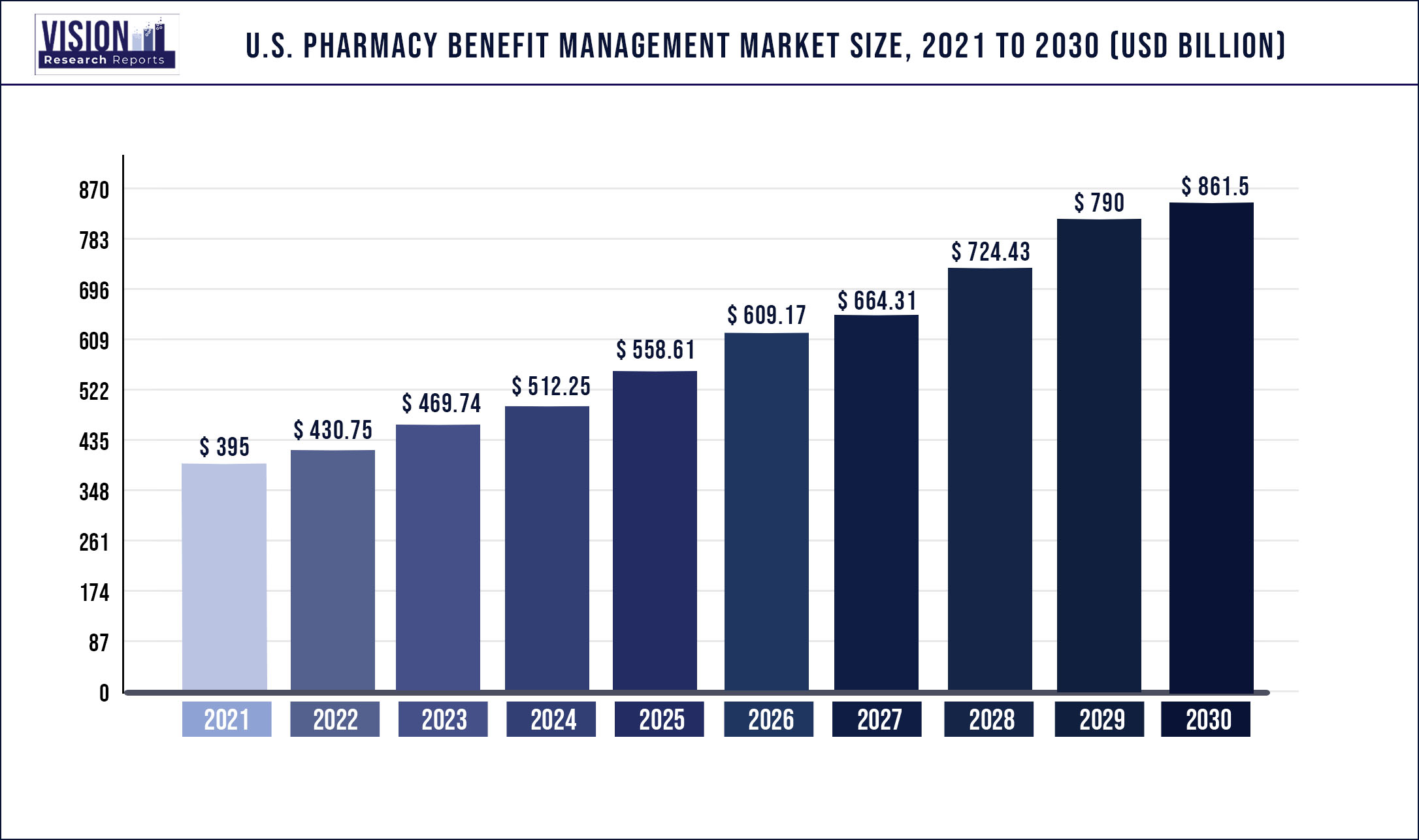
The U.S. pharmacy benefit management market size was estimated at USD 395 billion in 2021 and it is expected to surpass around USD 861.5 billion by 2030, poised to grow at a CAGR of 9.05% over the forecast period 2022 to 2030.
Increasing vertical integration of key market players, rising prevalence of chronic disease, and shrinking FDA generic-approval backlog are some of the primary growth stimulants for the market.
Vertical integration of pharmacy benefits management (PBM) organizations with health insurance companies are poised to result in increased control of PBMs over distribution systems. This will lead to rise in rebates, ultimately increasing the cost of drug list prices. Moreover, it will result in a monopoly of certain market player, concentrating sales and revenue generation.
The business of insuring and administering employee benefit programs in the country, especially, health care programs, is heavily regulated by federal and state laws and administrative agencies, such as the Department of Health and Human Services (HHS), State Departments of Insurance, Centers for Medicare & Medicaid Services (CMS), Internal Revenue Services, and Departments of Labor.
All PBM businesses in the U.S. must include home delivery and specialty pharmacies licensed as pharmacies in the states of establishment. Several states in the country regulate the scope of prescription (Rx) drug coverage and delivery channels to receive drugs for managed care organizations (MCOs), insurers, and Medicaid care plans. Certain home delivery and specialty pharmacies must be registered with the U.S. Drug Enforcement Administration (DEA) and individual state controlled substance authorities.
Scope of the Report
| Report Coverage | Details |
| Market Size in 2021 | USD 395 Billion |
| Revenue Forecast By 2030 | USD 861.5 Billion |
| Growth Rate from 2022 to 2030 | CAGR of 9.05% |
| Base Year | 2021 |
| Forecast Period | 2022 to 2030 |
Business Model Insights
Standalone pharmacy benefits management held the leading revenue share in the market in 2021. It included major players such as CVS Health and Express Scripts who underwent major mergers by the end of 2021. The merger trend was introduced recently in this market as the Federal Trade Commission (FTC) refused many applications for mergers in the past, mainly between pharmaceutical players and PBMs.
The mergers were anticipated to allow drug manufacturers to manage pricing policies and to understand pricing information of competitors. However, the market experienced consolidations between PBMs and health insurers leading to the strengthening of key players in the market. Key mergers will be effective from 2020 along with other agreements and alliances that will change market dynamics over the forecast period.
End-Use Insights
Based on end-use, the U.S. PBM market has been bifurcated into commercial and federal. The commercial segment is anticipated to dominate the market throughout the forecast horizon. The majority of the U.S. employees are enrolled under commercial private insurance plans to benefit from the copay system for high-cost drugs.
Federal support is significant for government employees wherein premiums vary for different health plans and are paid in part by employers and employees. Employers usually pay up to 72.0% of the total amount in an average plan for self-only or family coverage while employees pay the rest.
Key Players
Market Segmentation
By Business Model
By End User
Chapter 1. Introduction
1.1. Research Objective
1.2. Scope of the Study
1.3. Definition
Chapter 2. Research Methodology
2.1. Research Approach
2.2. Data Sources
2.3. Assumptions & Limitations
Chapter 3. Executive Summary
3.1. Market Snapshot
Chapter 4. Market Variables and Scope
4.1. Introduction
4.2. Market Classification and Scope
4.3. Industry Value Chain Analysis
4.3.1. Raw Material Procurement Analysis
4.3.2. Sales and Distribution Channel Analysis
4.3.3. Downstream Buyer Analysis
Chapter 5. COVID 19 Impact on U.S. Pharmacy Benefit Management Market
5.1. COVID-19 Landscape: U.S. Pharmacy Benefit Management Industry Impact
5.2. COVID 19 - Impact Assessment for the Industry
5.3. COVID 19 Impact: Global Major Government Policy
5.4. Market Trends and Opportunities in the COVID-19 Landscape
Chapter 6. Market Dynamics Analysis and Trends
6.1. Market Dynamics
6.1.1. Market Drivers
6.1.2. Market Restraints
6.1.3. Market Opportunities
6.2. Porter’s Five Forces Analysis
6.2.1. Bargaining power of suppliers
6.2.2. Bargaining power of buyers
6.2.3. Threat of substitute
6.2.4. Threat of new entrants
6.2.5. Degree of competition
Chapter 7. Competitive Landscape
7.1.1. Company Market Share/Positioning Analysis
7.1.2. Key Strategies Adopted by Players
7.1.3. Vendor Landscape
7.1.3.1. List of Suppliers
7.1.3.2. List of Buyers
Chapter 8. Global U.S. Pharmacy Benefit Management Market, By Business Model
8.1. U.S. Pharmacy Benefit Management Market, by Business Model, 2022-2030
8.1.1. Standalone PBM
8.1.1.1. Market Revenue and Forecast (2017-2030)
8.1.2. Health Insurance Providers
8.1.2.1. Market Revenue and Forecast (2017-2030)
8.1.3. Retail Pharmacy
8.1.3.1. Market Revenue and Forecast (2017-2030)
Chapter 9. Global U.S. Pharmacy Benefit Management Market, By End User
9.1. U.S. Pharmacy Benefit Management Market, by End User, 2022-2030
9.1.1. Commercial
9.1.1.1. Market Revenue and Forecast (2017-2030)
9.1.2. Federal
9.1.2.1. Market Revenue and Forecast (2017-2030)
Chapter 10. Global U.S. Pharmacy Benefit Management Market, Regional Estimates and Trend Forecast
10.1. North America
10.1.1. Market Revenue and Forecast, by Business Model (2017-2030)
10.1.2. Market Revenue and Forecast, by End User (2017-2030)
10.1.3. U.S.
10.1.3.1. Market Revenue and Forecast, by Business Model (2017-2030)
10.1.3.2. Market Revenue and Forecast, by End User (2017-2030)
10.1.4. Rest of North America
10.1.4.1. Market Revenue and Forecast, by Business Model (2017-2030)
10.1.4.2. Market Revenue and Forecast, by End User (2017-2030)
10.2. Europe
10.2.1. Market Revenue and Forecast, by Business Model (2017-2030)
10.2.2. Market Revenue and Forecast, by End User (2017-2030)
10.2.3. UK
10.2.3.1. Market Revenue and Forecast, by Business Model (2017-2030)
10.2.3.2. Market Revenue and Forecast, by End User (2017-2030)
10.2.4. Germany
10.2.4.1. Market Revenue and Forecast, by Business Model (2017-2030)
10.2.4.2. Market Revenue and Forecast, by End User (2017-2030)
10.2.5. France
10.2.5.1. Market Revenue and Forecast, by Business Model (2017-2030)
10.2.5.2. Market Revenue and Forecast, by End User (2017-2030)
10.2.6. Rest of Europe
10.2.6.1. Market Revenue and Forecast, by Business Model (2017-2030)
10.2.6.2. Market Revenue and Forecast, by End User (2017-2030)
10.3. APAC
10.3.1. Market Revenue and Forecast, by Business Model (2017-2030)
10.3.2. Market Revenue and Forecast, by End User (2017-2030)
10.3.3. India
10.3.3.1. Market Revenue and Forecast, by Business Model (2017-2030)
10.3.3.2. Market Revenue and Forecast, by End User (2017-2030)
10.3.4. China
10.3.4.1. Market Revenue and Forecast, by Business Model (2017-2030)
10.3.4.2. Market Revenue and Forecast, by End User (2017-2030)
10.3.5. Japan
10.3.5.1. Market Revenue and Forecast, by Business Model (2017-2030)
10.3.5.2. Market Revenue and Forecast, by End User (2017-2030)
10.3.6. Rest of APAC
10.3.6.1. Market Revenue and Forecast, by Business Model (2017-2030)
10.3.6.2. Market Revenue and Forecast, by End User (2017-2030)
10.4. MEA
10.4.1. Market Revenue and Forecast, by Business Model (2017-2030)
10.4.2. Market Revenue and Forecast, by End User (2017-2030)
10.4.3. GCC
10.4.3.1. Market Revenue and Forecast, by Business Model (2017-2030)
10.4.3.2. Market Revenue and Forecast, by End User (2017-2030)
10.4.4. North Africa
10.4.4.1. Market Revenue and Forecast, by Business Model (2017-2030)
10.4.4.2. Market Revenue and Forecast, by End User (2017-2030)
10.4.5. South Africa
10.4.5.1. Market Revenue and Forecast, by Business Model (2017-2030)
10.4.5.2. Market Revenue and Forecast, by End User (2017-2030)
10.4.6. Rest of MEA
10.4.6.1. Market Revenue and Forecast, by Business Model (2017-2030)
10.4.6.2. Market Revenue and Forecast, by End User (2017-2030)
10.5. Latin America
10.5.1. Market Revenue and Forecast, by Business Model (2017-2030)
10.5.2. Market Revenue and Forecast, by End User (2017-2030)
10.5.3. Brazil
10.5.3.1. Market Revenue and Forecast, by Business Model (2017-2030)
10.5.3.2. Market Revenue and Forecast, by End User (2017-2030)
10.5.4. Rest of LATAM
10.5.4.1. Market Revenue and Forecast, by Business Model (2017-2030)
10.5.4.2. Market Revenue and Forecast, by End User (2017-2030)
Chapter 11. Company Profiles
11.1. CVS Health
11.1.1. Company Overview
11.1.2. Business Model Offerings
11.1.3. Financial Performance
11.1.4. Recent Initiatives
11.2. Aetna
11.2.1. Company Overview
11.2.2. Business Model Offerings
11.2.3. Financial Performance
11.2.4. Recent Initiatives
11.3. Express Scripts
11.3.1. Company Overview
11.3.2. Business Model Offerings
11.3.3. Financial Performance
11.3.4. Recent Initiatives
11.4. Cigna
11.4.1. Company Overview
11.4.2. Business Model Offerings
11.4.3. Financial Performance
11.4.4. LTE Scientific
11.5. OptumRx, Inc.
11.5.1. Company Overview
11.5.2. Business Model Offerings
11.5.3. Financial Performance
11.5.4. Recent Initiatives
11.6. Walgreens Booth Alliance
11.6.1. Company Overview
11.6.2. Business Model Offerings
11.6.3. Financial Performance
11.6.4. Recent Initiatives
11.7. MedImpact Healthcare Systems, Inc.
11.7.1. Company Overview
11.7.2. Business Model Offerings
11.7.3. Financial Performance
11.7.4. Recent Initiatives
11.8. Anthem
11.8.1. Company Overview
11.8.2. Business Model Offerings
11.8.3. Financial Performance
11.8.4. Recent Initiatives
11.9. Rite Aid
11.9.1. Company Overview
11.9.2. Business Model Offerings
11.9.3. Financial Performance
11.9.4. Recent Initiatives
Chapter 12. Research Methodology
12.1. Primary Research
12.2. Secondary Research
12.3. Assumptions
Chapter 13. Appendix
13.1. About Us
13.2. Glossary of Terms
 Cross-segment Market Size and Analysis for
Mentioned Segments
Cross-segment Market Size and Analysis for
Mentioned Segments
 Additional Company Profiles (Upto 5 With No Cost)
Additional Company Profiles (Upto 5 With No Cost)
 Additional Countries (Apart From Mentioned Countries)
Additional Countries (Apart From Mentioned Countries)
 Country/Region-specific Report
Country/Region-specific Report
 Go To Market Strategy
Go To Market Strategy
 Region Specific Market Dynamics
Region Specific Market Dynamics Region Level Market Share
Region Level Market Share Import Export Analysis
Import Export Analysis Production Analysis
Production Analysis Others
Others